Many people associate heart health with cholesterol, blood pressure, or exercise routines, but a growing body of research suggests that your liver may also play a critical role.
Nonalcoholic fatty liver disease, or NAFLD, affects nearly one in four adults in the United States.
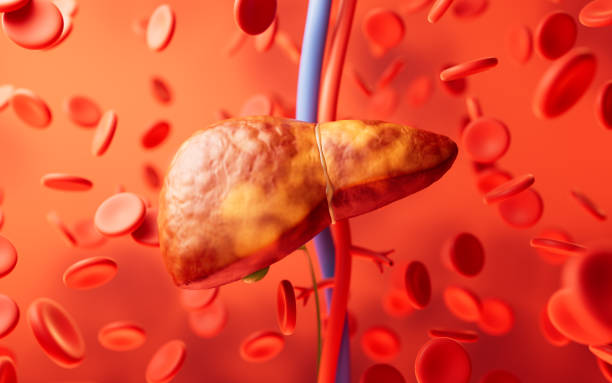
Unlike liver conditions linked to alcohol use, NAFLD occurs when fat builds up in the liver without alcohol being a factor.
While this condition is already known to increase the risk of liver damage and atherosclerosis, recent studies show a significant association between NAFLD and heart failure.
In an analysis of national health data between 2005 and 2018,
Researchers found that individuals with NAFLD were over three times more likely to have heart failure than those without the condition—even after adjusting for age, gender, and other factors
Heart failure, which affects about 6 million adults in the U.S., occurs when the heart is unable to pump blood effectively.
Although it cannot be cured, it can often be managed through medication, medical procedures, and lifestyle modifications.
The troubling link between NAFLD and heart failure highlights the need for a more integrated approach to care—one that considers liver health as part of the broader cardiovascular picture.
Obesity, diabetes, high cholesterol, and sedentary lifestyles are major contributors to both conditions.
By addressing these underlying factors early, you can reduce your risk for both liver and heart complications.
The American Heart Association recommends following its Life’s Essential 8 checklist, which includes maintaining a healthy weight, staying active, eating nutritious foods, and getting adequate sleep.
While lifestyle change may feel overwhelming, even small steps—like adding more fiber to your diet or taking regular walks—can have a cumulative and lasting impact.
It’s also important to recognize that NAFLD often has no obvious symptoms, making routine checkups and screenings essential.
A simple blood test or ultrasound can help your healthcare provider assess liver function and detect signs of fat accumulation early.
The earlier NAFLD is diagnosed, the more effectively it can be managed, often with non-invasive interventions like dietary improvements and weight loss.
In addition to medical evaluations, awareness and education are vital.
A recent video from the Cleveland Clinic breaks down the relationship between metabolic health and liver function, illustrating how lifestyle adjustments can reverse early stages of NAFLD.
For those already managing heart failure or chronic conditions like diabetes, regular communication with your doctor can ensure that liver markers are being monitored alongside cardiovascular health.
This dual focus can help identify potential complications earlier and guide more targeted treatment.
The connection between liver fat and heart strain may be underrecognized, but it is not insignificant.
Bringing liver health into the heart health conversation empowers both patients and providers to take more proactive, preventive steps.
It serves as a reminder that your body’s systems do not function in isolation—what impacts one organ often has ripple effects throughout the body.
By staying informed, getting regular screenings, and making thoughtful lifestyle choices, you can support your liver, protect your heart, and feel more in control of your long-term health.